Precision and Innovation: Insights on a robust radiation oncology practice from a long-term CyberKnife® System user
Introduction
According to the World Health Organization, in 2050 more than 35 million new cancer cases will be diagnosed, a 77 percent increase from the estimated 20 million cases in 20221. Men are anticipated to be the hardest hit, with a study in the journal Cancer finding that global cancer cases are expected to increase by 84 percent in this timeframe and deaths expected to increase by 93 percent2.
The news isn’t entirely grim, however. Practitioners around the globe and in the U.S., specifically, have more options than ever for treating cancer and it’s anticipated that new modalities will continue to be introduced as science and technology evolve.
Radiation therapy is a critical treatment option at multiple points in the cancer care continuum. In fact, in 2024, it is estimated that more than one million U.S. cancer patients will receive treatment with radiation therapy3. The radiation oncology team is key to the successful care of cancer patients and with the right resources, have the opportunity to expand their referral base and the number of people they can help.
Leveraging the CyberKnife® System, clinicians can build a reputation in their community as the go-to provider for exceptional patient care. This differentiated system combines advanced precision and real-time artificial intelligence (AI)-driven motion tracking and synchronization treatment delivery for all stereotactic radiosurgery (SRS) and stereotactic body radiation therapy (SBRT) treatments. The CyberKnife System provides care teams with tools to help them effectively treat a wide range of tumor types and the speed they need to support their busy practices.
Dr. Timothy A. Jamieson and his team have built a thriving radiation oncology practice at Southeast Georgia Health System’s Cancer Care Center & CyberKnife program in Brunswick, Georgia using the CyberKnife System with Synchrony® and the VOLO™ Optimizer. He shares his perspective on the use of SBRT and insights into how their facility has achieved a significant growth in annual CyberKnife System patient volume.
Overview
The team began treating patients in 2011 with an early model of the CyberKnife platform and six years later upgraded to the CyberKnife M6 System, with subsequent software enhancements including the Accuray Precision® Treatment Planning System with the new VOLO Optimizer, and the addition of the Incise® Multi-leaf Collimator. During the first full year of operation 200 people received care and as of 2024, the team is treating 600-700 people per year.
There has been a steady increase in patient numbers based on 1) expansion of the types of cases treated, 2) focus on SBRT as a competitive differentiator, 3) an increase in referring physicians, and 4) the introduction of targeted local marketing.
The top four indications treated by the Brunswick team, accounting for about 95 percent of cases, are prostate, lung, and breast cancers, and oligometastatic diseases. With the launch of the CyberKnife System the team focused on the treatment of prostate cancer. Almost all prostate cancer patients, including node positive, but not men who have previously had a prostatectomy, are treated in five fractions on the CyberKnife System. While prostate cancer is still the number one tumor type treated, there has been a rapid increase in the number of people with stage 1 lung cancer receiving radiation therapy.
The introduction of the low dose CT scan screening program resulted in the identification of significantly more stage 1 lung tumors. The center developed a very active pulmonology program using navigational bronchoscopy that is very effective at performing biopsies in peripheral lung tumors, and at the same time placing fiducial markers, making it easier to treat patients with radiation and laying the foundation for substantial growth in the lung radiosurgery program.
The third most frequently treated indication is stage 1 breast cancer and ductal carcinoma in situ (DCIS). For Dr. Jamieson, the system offers a much tighter field, treating strategically around the area at risk to minimize the dose to healthy tissue and in the same time as treating a traditional field with a traditional regimen. More than half of these tumors are currently treated with five-fraction SBRT delivered using the CyberKnife System and Dr. Jamieson expects the types of breast related tumors that can be treated with the system to continue to expand.
The fastest rising treatment area is oligometastatic disease, particularly for those with primary disease of the prostate, with the advent of PSMA PET scans which has significantly improved the detection of this type of cancer. Men identified with metastatic lesions are typically treated with three to five fractions on the CyberKnife System.
The software enhancements on the CyberKnife System, including Synchrony and Accuray Precision Treatment Planning System with the VOLO optimizer, have increased the speed with which Dr. Jamieson and his team plan and treat various indications. With an 8:30-4pm workday, the center is able to treat 600-700 people per year with these tumor types.
The radiation therapy department consists of an Accuray CyberKnife System, a Varian TrueBeam and an HDR brachytherapy device. Conventional cases are treated with the TrueBeam and SBRT cases with the CyberKnife System.
The staff consists of three physicians, two physicists, two remote dosimetrists, six therapists, two CyberKnife System coordinators who are former therapists, and a nurse practitioner who focuses full time on people treated with the system. One of these coordinators was recently converted to the coordinator role to manage the busy practice.
The Economics of SBRT
One of the reasons some practices aren’t currently prioritizing SBRT is because nine weeks of IMRT in the U.S. will generate more revenue than one week of SBRT, but one of the key advantages of the CyberKnife System is the ease and precision of delivering highly precise SBRT treatments.
From Dr. Jamieson’s perspective, while he is paid less per patient with a five-fraction regimen he treats more patients overall, and his throughput is “enormous.” Instead of maximizing his per patient revenue he focuses on his total revenue, and that’s why he is able to treat 600-700 patients per year with their CyberKnife System and 300-400 using their TrueBeam. Additionally, with SBRT, Dr. Jamieson has noticed that his team has a more predictable, regular workday and fewer therapists are required. Patients benefit because they can begin treatment more quickly, there isn’t a backlog of people requiring up to six weeks of care.
Five-fraction SBRT is delivered with sub-millimeter precision and accuracy, and also causes less disruption of patients’ daily lives, enabling improved treatment compliance for those people who are unable to travel a month or more for conventional radiation therapy.
Dr. Jamieson also believes that if an alternative payment model is approved and there is a fixed reimbursement based on a diagnosis, more doctors will move to treating patients with SBRT. He believes that doctors will “realize that we can do this in one week. We’re going to make the same amount of money and get patients through their treatment faster. There will be more of an emphasis on the patient and the impact of treatment on them, and the data, and doctors will get rewarded by having more patients as opposed to maximizing revenue on each individual patient.”
The Business of SBRT
The majority of Dr. Jamieson’s patients – about 85 percent – are local, coming from referring network physicians including urologists, pulmonologists and breast surgeons and those in surrounding towns an hour or two away. These are specialists who understand the value of radiation therapy, are comfortable referring patients for treatment, and have happy patients returning to them following their treatments.
Initially, when establishing a referral network, Dr. Jamieson believes he could have done a better job anticipating the wariness of other doctors and their concerns about losing the procedure and control of the patient, along with their skepticism related to new technology. He notes that these concerns tend to take care of themselves when patients return to their doctor and are happy, but that takes time. Making an effort to help doctors feel comfortable earlier in the process of developing a referral base can help speed up the timeline.
Also, Dr. Jamieson would have pushed to establish a referral network connected to a lung cancer screening program before it launched to the public and advocated for patient education to drive uptake. This type of screening has the potential to identify a lot of stage 1 lung tumors that often can be treated with radiation. The first few years of the hospital’s program – without the network – Dr. Jamieson’s team didn’t see many patients, which was a lost opportunity.
The remaining 15 percent of their business is driven by marketing through a combination of their team’s and the hospital’s efforts. They primarily rely on podcasts, rotary talks and website content highlighting patient experiences, with newspaper and radio ads in towns that are outside their immediate vicinity.
Dr. Jamieson and his team are also doing an increasing number of telehealth consultations with people who live outside of Brunswick and based on what they’ve read on the facility’s website, want to have an appointment via telehealth. It enables the patient to learn more about the CyberKnife System without committing time and resources to drive to the clinic. Dr. Jamieson believes if he and his team would have put more time into identifying a systematic approach for raising awareness and scheduling telehealth consults, they could have greatly expanded beyond their current patient base.
Advice
Dr. Jamieson has the following words of advice for other medical professionals interested in starting – or growing – their CyberKnife System program.
First, the radiation oncologist(s) has to believe in SBRT. They have to be an advocate or it’s not going to work. If the doctors running the program don’t believe in it, it’s not going to be successful.
Secondly, they need to curate the referral base and that’s both a push and a pull in terms of training. Because referring doctors are critical to the success of a CyberKnife System program, marketing to them and locally within the community to really drive patient volumes will be key.
Accuray Tools to Help Expand Clinical Practices
Three decades of real-world experience and more than 5,000 publications support the use of the CyberKnife System. Since its introduction, innovative new technology has been introduced to enhance treatment planning and delivery. Dr. Jamieson, along with clinicians worldwide, have adopted advanced functionality on their CyberKnife System to facilitate the delivery of precise treatments for more patients each day.
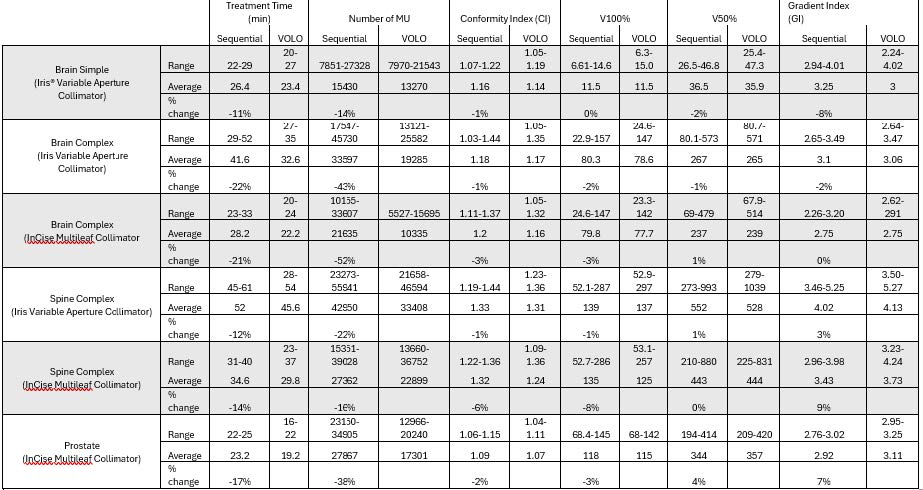
The latest Accuray Precision® Treatment Planning System (TPS) with the VOLO™ Optimizer significantly reduces the time required to create high-quality treatment plans and to deliver them, making patient treatments much faster compared to earlier TPS versions. VOLO cuts optimization time by up to 90% and enhances plan quality, enabling treatments to be delivered up to 50% faster4. A 2019 study found VOLO was superior for target coverage for prostate and spine, and for brain and for urethra dose minimization as compared to a previous sequential optimization algorithm. This study also reported that for MLC-based plans the VOLO Optimizer produced significantly better dose distribution for brain metastases compared to the earlier sequential optimizer5.
Another study found that the VOLO optimizer maintains and improves the plan quality while decreasing the complexity compared to the earlier sequential TPS. This was evident in the reductions of treatment time, number of beams used and in the number of monitor units delivered. This has facilitated the potential to increase patient load without decreasing the quality of the treatment plan6.
Artificial intelligence (AI)-driven Synchrony® is the only technology that uses continual image guidance to automatically adapt the movement of the radiation beam in synchronization with the movement of the tumor. The Synchrony software is designed to provide highly precise radiation dose delivery to tumors that move, such as lung and prostate, and smaller, tighter treatment margins around the tumor, helping to minimize the amount of healthy tissue exposed to high-dose radiation. The beams of radiation are delivered continuously throughout the treatment session as the patient breathes naturally. In comparison, gating methods deliver radiation only when the tumor is close to the expected location and pause treatment delivery when the moving tumor is outside of the “treatment window.” This potentially lengthens the treatment time and therefore can compromise clinical efficacy, and patient comfort.
Dr. Jamieson, in his own words, is extremely SBRT centric. He believes you have to be, to have a busy CyberKnife System center. “You’ve got to look for indications to be treated with SBRT first and then find a reason why you wouldn’t do it.” In his mind, a CyberKnife System and a traditional machine are very complementary. While other radiation therapy devices can deliver SBRT, Dr. Jamieson believes the CyberKnife System has a definite advantage over a conventional linear accelerator in terms of its ability to correct for motion and maintain sub-millimeter accuracy and precision. Ultimately it helps to expand and enhance what a center can offer patients, while also improving the center’s business model.
REFERENCES
1 World Health Organization February 2024 press release.https://www.who.int/news/item/01-02-2024-global-cancer-burden-growing–amidst-mounting-need-for-services. Accessed on April 21, 2025
2 Bizuayehu HM, Dadi AF, Ahmed KY, et al. Burden of 30 cancers among men: global statistics in 2022 and projections for 2050 using population-based estimates. Cancer. 2024; 130(21): 3708-3723. doi:10.1002/cncr.35458
3 Calculation based on information found on the American Cancer Society website: Cancer Facts & Figures 2025 (Excluding non-melanoma skin cancers, over 2 million new cancer cases are expected to be diagnosed in the US in 2025) https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2025/2025-cancer-facts-and-figures-acs.pdf. More than half of people with cancer get radiation therapy [https://www.cancer.org/cancer/ managing-cancer/treatment-types/radiation/basics.html] Access on April 21, 2025
4 Internal Accuray evaluation comparing the Accuray Precision TPS with CyberKnife VOLO Optimizer solution, to other TPS, either for CyberKnife or other radiation therapy systems.
5 Zeverino M, et al. Novel inverse planning optimization algorithm for robotic radiosurgery: First clinical implementation and dosimetric evaluation. Phys Med. 2019 Aug;64:230-237. doi: 10.1016/j.ejmp.2019.07.020
6 Schüler E, Lo A, Chuang CF, Soltys SG, Pollom EL, Wang L. Clinical impact of the VOLO optimizer on treatment plan quality and clinical treatment efficiency for CyberKnife. J Appl Clin Med Phys. 2020 May;21(5):38-47. doi: 10.1002/acm2.12851. Epub 2020 Mar 25. PMID: 32212374; PMCID: PMC7286021
The views contained and expressed, are those of the author and do not necessarily reflect the views or policies of Accuray Incorporated or its subsidiaries. No official endorsement by Accuray Incorporated or any of its subsidiaries of any vendor, products or services contained in this case study is intended or should be inferred.