Certainty
Matters.
Expand the curative power of radiation therapy to improve as many lives as possible.

Certainty
Matters.
Expand the curative power of radiation therapy to improve as many lives as possible.


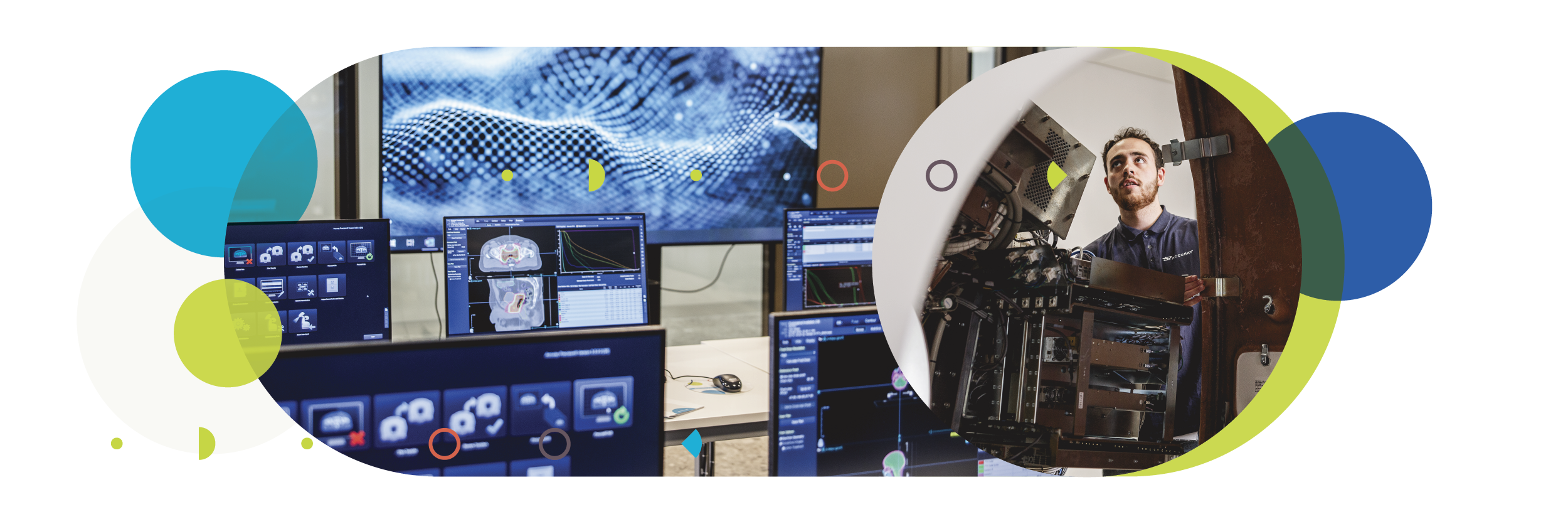
At Accuray, we are committed to designing radiotherapy solutions that can take on the most complex challenges — while making commonly treatable cases even easier. Our unique, market-changing solutions are designed to deliver radiation treatments across a full spectrum of patient needs, with a global reach that extends our innovative practices worldwide. Our commitment to continued innovation aims to enhance care, improve quality of life, and address diverse healthcare needs around the globe.
systems installed
Treatment systems in
revenue invested in R&D
Efficiency of
Care
Provide radiation therapy treatments in a simple, fast and seamless workflow.
Confidence in Care
Deliver radiation therapy with confidence in a rapidly evolving field.
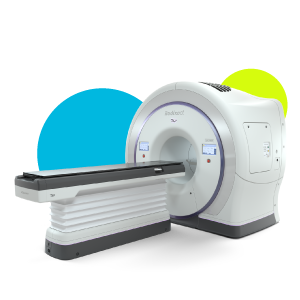
CyberKnife® S7™

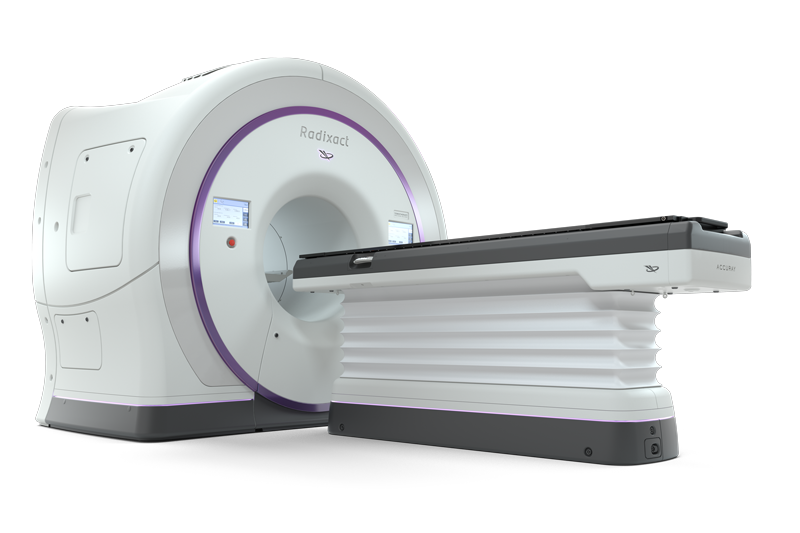
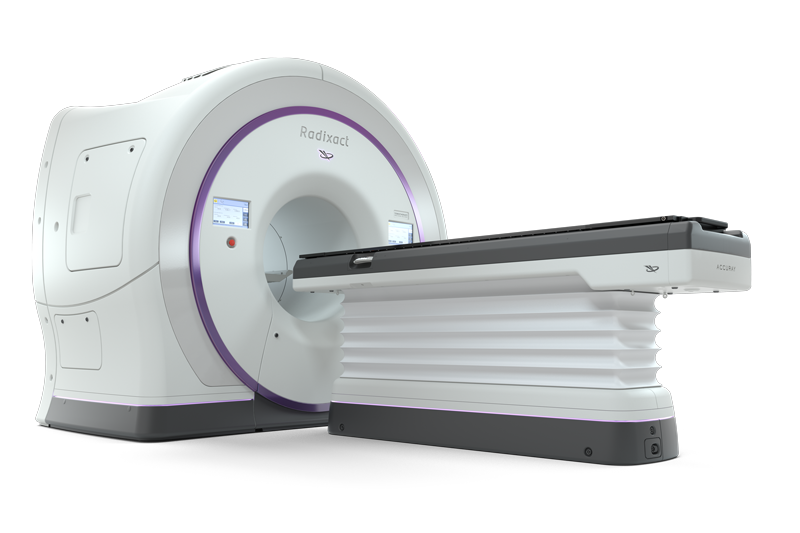
Radixact®
Expands patient-first treatment like no other system in the world
CyberKnife® S7™

Radixact®

Join our thriving Accuray users’ community, gaining free access to a platform to connect with peers, exchange experiences, and keep up-to-date with news and developments in your field. You’ll also have access to a wide range of training opportunities to ensure you stay informed about the latest advancements. Connect, exchange, and learn with us.
What's new
Talk with an
Accuray Expert